![]()
A History of Western Medicine, Medical Progress and Advances
An excerpt from the book titled Slaughter of the Innocent by medical historian Hans Ruesch, CIVITAS Publications, Hartsdale NY, 1979 and 1991, pages 147-200
A summary of how human medicine progressed due to scientific and ethical research and treatment of humans and was often led astray by unscientific methods that contributed to millions of injuries and deaths.
A preface note: Mr Ruesch's contributions to humanity were recognised in two books that recognise history's luminaries. Ruesch is honoured - alongside Orwell, Darwin, Shaw, Plato, Sartre, Aristotle, Keats, Carlyle, Herodotus, Hoyle, Ruskin and Flaubert, amongst others - in the 2002 book Past to Present: Ideas That Changed Our World by Terry and Stuart Hirschberg. That book includes fourteen pages of excerpts from Slaughter. He is also honoured in the 2003 book called Ideas that Changed the World by Felipe Fernandez-Armesto; listed alongside Einstein and Gandhi as inclusions from the 20th century. There are links to some articles about Mr Ruesch below this history of medicine.
- Hippocrates: Nature heals; Diet, Hygiene & Asepsis
- Galen & Vivisection - Loss of Hygiene & Asepsis; the Descent into 1500+ Years of Plague
- Human Anatomy - Vesalius
- Circulation of the Blood: Harvey & Da Vinci
- The Microscope & Germs: Leeuwenhoek & Spallanzani
- Nutrition & Diet eg. Scurvy and Vitamin C
- Diagnostics: Percussions and Auscultation
- Heart Disease & Digitalis
- Asepsis, Antiseptic Surgery & Iodine
- Quinine and Malaria
- Vaccination & Innoculation
- Surgery: Rediscovery of Methods, Anaesthesia, Hygiene & Asepsis
- Anaesthesia: Conquering Pain
- Rediscovery of Surgical Hygiene & Asepsis: Semmelweis
- Surgical Training
- Blue Babies
- Germ Theory, Vaccines & Other Confusions
- Germ Theory
- Rabies vaccine
- Tuberculosis & the Tuberkulin Disaster
- Cholera
- Diseases that came and went without any vaccination
- Smallpox Vaccination
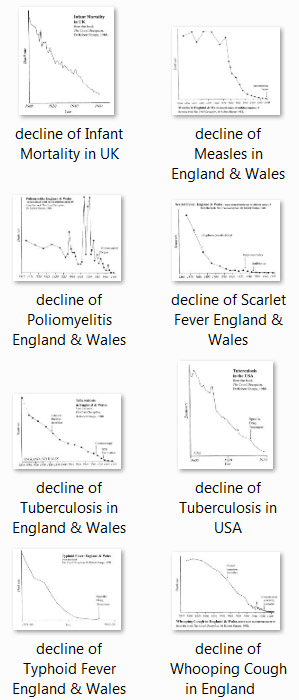
- Hygiene: The Decline of the Infectious Diseases
- Polio: Salk Vaccine
- Life Expectancy
Hippocrates: Nature heals; Diet, Hygiene & Asepsis.
Hippocrates is considered the greatest physician of antiquity and some consider him the greatest of modern times as well. Ever stronger currents today point toward a return to Hippocratic principles and wisdom, which Greece had probably adopted from Persia and India, where medical art and surgical science had always been very advanced.
Hippocrates lived in the 5th Century B.C., and all historians agree that he taught validly concerning epidemics, fever, epilepsy, fractures, the difference between malignant and benign tumours, health in general, and most of all the importance of hygiene, the healing power of food and the need for high ethical values in the practice of medicine. A great clinician, he would observe the patient attentatively and then help him to be cured by vis suprema guaritrix: Nature, the Supreme Healer. He laid utmost stress on hygiene and diet, but used herbal remedies and surgery when necessary...
Henry E. Sigerist, who held the Chair of the History of Medicine at the Universities of Leipzig and Johns Hopkins, and whom many consider the outstanding medical historian of our time, describes Hippocrates' medical philosophy thus:
"Nature heals. The doctor's task consists in strengthening the natural healing powers, to direct them, and especially not to interfere with them. The dietetic treatment is the best. Through the food the power regenerates itself. Hippocratic dietetics reached a level that to our day merit our great admiration." (Grosse Aerzte, 6th Edition, Lehman, Munich, 1969, p.28)
In another of his medical works, Krankheit und Zivilisation (A.Metzner, Frankfurt, 1952, p. 237) Sigerist states: "The dietetical prescriptions which the Hippocratic doctors elaborated for their patients are the same that are being prescribed today."
Not much reasoning power is needed to understand that the same diet that helps to restore a patient's health will also keep a healthy person physically sound - today no less than in Hippocrates' day.
But only today do we fully realize how valuable Hippocrates' teachings were, based solely on his clinical observation and true medical intuition. So we know from operations and autopsies that a liver which has been ruined and scarified by wrong alimentary habits can regenerate itself completely - provided the damage is not too great - in a comparatively short time (1-2 years) of proper diet, whereas the intake of "little liver pills" is bound to worsen the condition, poisoning the organism still further. When today a drug-swallowing hepatic patient recovers, it is in spite of the drugs, if luckily they are ineffective, and not because of them.
Historian Sigerist, having been formed at the conventional medical schools of France, Switzerland and the U.S., was not an anti-vivisectionist, so he can hardly be suspected of anti-vivisectionist bias when he wrote of the man he regarded as the greatest doctor of our time, Germany's doctor August Bier, the inventor of lumbar anaesthesia:
"After 1920, Bier turned his back entirely on individual experimentation. To his mind it is a mistake to believe that today's medical art has reached a higher level than ever before, and he called for the establishment of a completely new medical system. The true medical art has declined, having been overshadowed by laboratory research. The sense and understanding of the whole has been lost, the result of experiments is being extrapolated to man without any critical sense ... frog and rabbit say nothing ... Medicine is lucky to have in Hippocrates a great paradigm. We must return to a true medical concept, to the "clinical outlook". (Grosse Aerzte, p.436)
The March 20, 1904, Paris edition of the New York Herald Tribune brought opinions of dozens of well-known doctors, all anti-vivisectionists, including the following of a Dr. Salinas: "Hippocrates never vivisected, and yet he raised medical art to a level from which we are very far today, in spite of the alleged great modern discoveries."
All historians have ascribed to Hippocrates a very high ethical sense, which is irreconcilable with vivisectionist practices. It is not by coincidence that the physician's oath bears Hippocrates' name and not Galen's.
Galen & Vivisection - Loss of Hygiene & Asepsis; the Descent into 1500+ Years of Plague.
Galen (130 - 200 AD) was a passionate vivisector and the first physician on record to demonstrate the danger of animal experimentation for medical science. His vivisection of animals did not merely fail to teach him anything about the human body, but became the source of grievous mistakes that were to wreak havoc on mankind for 15 centuries. All his valid knowledge came from his clinical experience [from his contact with patients] - how to set broken bones, for instance, and the therapeutic value of certain herbs.
Galen was thirty years old when he came to Rome from his native Pergamon in Greece, where he had already gained a reputation as the doctor to the gladiators, and in the next thirty years he was to become the the personal physician to five Emperors.
He was also a prolific writer on the medical art, and his monotheistic ideals, his belief in one supreme being, led the Catholic Church later on to decree his scientific doctrine as the only "correct" one. For various centuries, whoever dared raise doubts about a Galenic teaching was made to recant on the rack of the Holy Inquisition. As a consequence, humanity had to suffer for fifteen centuries from many fatal mistakes.
In 192 AD, a fire destroyed most of Galen's personal library, which included 400 of his medical treatises. Had the fire destroyed them all we would have to believe meekly the traditional teachings that describe Galen as the greatest medical man of antiquity. But the fire spared 98 of his medical works; and from them it emerges that all his valid medical knowledge came from his clinical experiences, from his contact with patients - like his belief that the mind influences organic reactions; whereas all his major errors derived from his vivisectioning of animals. He had a vast knowledge of herbs, like all Greek doctors, who had imported this knowledge from Asia.
In the course of time, the humane and hygienic precepts of Hippocrates were scorned. Plinius tells us that up to the First Empire the Romans had been a healthy people, thanks to the prevalent hygiene and sanitary services, exemplified by the aquaducts and the public thermae. But by and by, the reasonable Hippocratic precepts, such as intake of a frugal, simple diet, and rigorous cleanliness, which could be had for nothing, lost their fascination as a new breed of medical men discovered there was more money in preaching the importance of amulets, magic and astrology.
Not only in the Orient and ancient Egypt, but also in the Roman Empire, surgery had been highly developed. Operations performed in antiquity included tonsilectomies, removal of cataracts and goiters, trepanation of the cranium, the excision of tumors, the removal of kidney and gall stones, even plastic surgery. Celsus, the anti-vivisectionist Roman best qualified for the title of original scientist, and a follower of the Hippocratic school, had described many of these operations in a First Century manual on surgery.
But in the following centuries the gradual abandonment of Hippocratic hygiene, not yet known as asepsis, started increasing the danger of surgical operations to such an extent that little by little they were reduced to a minimum.
In the Middle Ages they were confined mostly to amputations, which were performed only in extreme cases, owing to the almost inevitable danger of infection and the difficulty of checking hemorrhages. The technique of the Greeks to ligature the vessels had gone the way of all surgical science, and the stumps were cauterized with red-hot irons or boiling oil.
Many of Galen's teachings were disastrous for mankind - such as his belief that pus was beneficial to healing, or that fruit is harmful. Galen had noticed that dogs and cats shunned fruits, and it was to be medieval man's misfortune that Galen's father, who never touched fruit, lived to an advanced age, so Galen saw in this a confirmation that the avoidance of fruit insures old age.
These and other Galenic mis-teachings made themselves tragically felt throughout the Middle Ages. The teachers of anatomy had no other texts than Galen's: woman has two wombs, one for the male children, the other for the females; urine is secreted directly from the vena cava. The blood passes from the right ventrical to the left ventrical through invisible pores. Galen had acquired all these and many other wrong notions either through his experiments on live animals, or in spite of them.
And his many vivisections had failed to reveal to Galen that the blood circulates, although he investigated the problem. In fact he is credited with the discovery that the veins do not contain air, as his contemporaries believed, but blood.
The abandonment of hygiene as an old-fashioned, pagan superstition was welcomed by the Church, owing to her horror of sex and nudity, and was fostered by her with dire consequences for mankind. Not only were the classic Greek and Roman images and statues of nudes destroyed, clad or painted over in most of Europe, but the public thermae that had done so much to keep the ancient Greek and Roman people healthy, were closed down. Body washing and even just looking at one's own nudity were considered evidence of sinfulness and depravity, and the few people who were sometimes ordered by their physician to take a bath were lowered into the tub fully clothed. To this day, for the rare baths in some Italian parochial boarding schools, a chaste bathing suit must be worn in the tub, and mirrors are absent.
All the medical historians (Sigerist, Dubos, Inglis) concur that the disappearance of the great medieval epidemics [infectious diseases] , including the bubonic plague which wiped out nearly half of Europe, was not due to the introduction of any specific therapy, but to the introduction of hygiene, of the sewer system and clean water in the cities, and that the startling improvements these institutions brought, raising life expectancy dramatically, started half a century before large-scale vaccination was adopted.
Oddly enough, it did not seem to occur to any of those historians that what they defined as the "mysterious" insurgence of those epidemics, was not mysterious at all but the inevitable consequence of Church-supported Galenism, i.e. the abandonment of Hippocratic hygiene.
The disastrous plagues of the Middle Ages were the legitimate offspring of the sad, long-lasting union between the sexuophobia of the Church and the extrapolation to man of observations made on animals, which, for instance, don't need washing with lots of soap and hot water after bringing forth, because the antiseptic effect of their own saliva is sufficient to prevent puerperal fever. Today, pestilences keep turning up wherever populations are crowded and cleanliness is absent. In unhygienic southern Italy, puerperal fever causes as many deaths as a century ago.
The ancient Greeks and Romans, who considered it normal to blind the rebels, impale the enemy soldiers and put to the sword the vanquished populations, had forbidden under pain of death, the section of human cadavers - but not of living animals; and later on the Church retained that attitude. This explains why in the Western world the medical men who were trying, like today's vivisectors, "to discover the secrets of human life" by cutting up living animals, moved backwards instead of forward, forgetting Hippocrates' teachings and getting morassed deeper and deeper in a Galenism seasoned with astrology, magic and religion. And then, as now, the majority went along, unthinkingly.
Human Anatomy - Vesalius
Some of the Greek culture and medical sciences that Europe had mislaid during the Middle Ages lived on and evolved in the East, as the Greek texts were translated into Syriac and from Syriac into Arabic. A few Oriental lights shone in the Medieval fog - in the 10th Century, Al Biruni, who came from central Asia, and who has been overlooked by the western historian, and in the following century Persia's Razes and the Arab Avicenna. But the great change was not to come until Martin Luther lifted the veils of obscurantism.
The first step out of the medical darkness was taken by Andreas Vesalius, a Belgian who since childhood had been cutting up live mice, cats and dogs and had declared the pig his favourite animal, for it never stopped grunting under his knife, while the other animals after a certain point stopped complaining.
His vivisections taught Vesalius nothing. It was only when he started dissecting the bodies of the hanged that he had stolen outside the walls of Luttich that he discovered Galen's errors, and published his findings in a treatise which is still considered a masterpiece of descriptive anatomy: De humani corporis fabrica, illustrated in Titian's workshop and published in Basil 1543.
But it was still dangerous to hint that Galen had erred. A few years earlier Paracelsus had lost his teaching position at the University of Basil for having publicly burned Galen's works; and his dismissal was demanded by the students themselves who worried about such disrespect of respected standards. And as late as 1560 an Englishman who wanted to be a doctor was asked first to recant the doubts he had expressed about Galen's teachings.
In fact Vesalius, who was teaching anatomy in Italy, at the University of Padua, could well have paid the penalty of heresy and been burnt alive at the stake, as was to happen ten years later to Miguel Servetus, the Spanish doctor-priest who had sectioned a cadaver; but Vesalius explained that he didn't want to contradict Galen but rather to demonstrate how accurate his descriptions had been - except for that venial little sin of assuming that what is true of a quadruped is also true of a man. However, the majority of the university brains, including his teacher Jakobus Sylvius, took their distance, accusing Vesalius of "heresy and folly". And Vesalius preferred to repair to Spain.
Truth had nevertheless started coming to light; but Galenism proved thick-skinned. Ignorance, especially the ignorance of the learned, has always been slow to die. For example, based on his observation of quadrupeds, Galen had described the human hipbone as being flared, like that of an ox. When Vesalius' book brought out the truth, the university teachers would not admit that they had perpetuated a millenarian error and explained that since Galen's day the human hipbone had changed shape owing to the habit of wearing pants instead of the toga.
It took almost two centuries after the publication of Vesalius' work to dissipate the last remnants of Galenic fog - but only to make room for another doctrine that was equally wrong and tyrannical, but far more harmful.
Circulation of the Blood - Harvey & Da Vinci
In 1628, less than a century after Vesalius' book, another famous work came out: the treatise on the circulation of the blood by William Harvey, an Englishman who had studied at Padua. The medical historians called him the "discoverer" of circulation, setting the blueprint for all the following historians, whose research usually consists in copying each other. And Harvey's alleged discovery was to become one of the battle horses of the vivisectionists.
That the blood circulates had been known for thousands of years. Even if Galen never knew it, the Orientals did. So already Nei Ching ("The Book of Medicine"), which form the basis of Chinese medical literatore, compiled in 2650 B.C. by scientist-Emperor Hwang Ti, included these words: "All the blood in the body is under the control of the heart ... . The blood current flows in a circle and never stops."
Not even today has all Oriental knowledge penetrated the West. Much less so in the Middle Ages. Suffice it to remember that Marco Polo, who introduced spaghetti from China to his native Italy, forgot to mention paper and printing, which the Chinese had been using for centuries.
Nevertheless, that the blood circulates wasn't a secret for the medieval scholars. Too many had already spoken about it. In the 13th Century the Arab Ibn an Nafis had written that the blood passes from the right side of the heart, through the lungs, to the left side. (His work was exumed from oblivion just before the Second World War.)
Another who knew about the circulation of the blood was Leonardo da Vinci, who for the sake of his art had studied the usual corpses of the hanged and discovered the function of many internal organs. In fact Leonardo rather than Vesalius would be considered the father of anatomical knowledge had his assistant who was to reproduce the drawings for the book he was preparing not died. Leonardo's original drawings are now scattered in many lands. Leonardo had already recognized that the basis of the two great arteries through which the blood issues from the heart are provided with valves that prevent the blood inverting its course and returning to the heart.
The question of the circulation of the blood evolved very slowly in the Western world because it was at odds with the "official" science of the day - with the opinion of Galen, according to which the blood was in a state of continual flux and reflux, like the ocean's tide. Also the heretic Servetus had explained in his Restitutio Christianismi that the blood passes from the right to the left side of the heart, and that in the course of this passage it got "refreshed" by something taken from the air: which is a quite accurate description of what actually happens. No wonder Harvey's claim to have discovered the circulation caused an immediate controversy.
It is clear that experiments on animals did not originate the theory that he [Harvey] propounded in his treatise, but experiments he made on corpses, and on himself. He made beautifully simple experiments on the living body by using his own arm and noticing on which side the blood accumulated. Thus he "discovered" what was already known, without the necessity of vivisecting animals. Then on the corpse of a man who had been hanged he forced water into first the right side of the heart and then the left, watching the direction and course of the fluid in each case. (Life and Works of William Harvey, Sydenham Society, Edited by Willis, p.507)
In his treatise, dedicated to the King of England, he couldn't admit that he had broken the law by experimenting on a human corpse, so he claimed to have come to his conclusions by vivisecting 80 different kinds of animals, a plainly ridiculous assertion. Once the principle was established, there would not have been much sense in going through the same motions with 80 different species. But it helped establish his reputation as as an earnest, thorough "scientist". Galen had kept vivisecting animals to "discover the truth" about the blood, and had come to wrong conclusions.
Lawson Tait, the greatest surgical innovator of modern times and foremost expert on medical science, went on record with a paper read on April 20, 1882, before the Philosophical Society, and had this to say about the question of Harvey's merits:
"Take the case of the alleged discovery of the circulation of the blood by Harvey, and it can be clearly shown that quite as much as Harvey knew was known before his time. That he made any solid contribution to the facts of the case by vivisection is conclusively disproved, and this was practically admitted before the Commission by such good authorities as Dr. Acland and Dr. Lauder Brunton. The circulation of the blood was not proved till Malpighi used the microscope, and though in that observation he used a vivisectional experiment, his proceeding was wholly unnecessary, for he could have better and more easily used the web of the frog's foot than its lung. It is, moreover, perfectly clear that were it encumbent on anyone to prove the circulation of the blood now as a new theme, it could not be done by any vivisectional method but could, at once, be satisfactorily established by a dead body and an injecting syringe. In fact, I think I might almost say that the systemic circulation was incompletely proved until the examination of injected tissues by the microscope had been made."
The Microscope & Germs - Leeuwenhoek & Spallanzani
Of true value to science was the invention of the microscope by Anthony Leeuwenhoek (1632 - 1723), a Dutch dry-goods store owner who liked to grind ever more powerful lenses in his spare time, until he became the first person who saw a unicellular organism - today named microbe, by means of an instrument that today we call microscope.
The Dutchman hadn't been dead long when in Italy Lazzaro Spallanzani was born (1729), who became a university professor at Reggio and Pavia. Although he was a priest, he was an indefatigable experimenter in every field, including vivisection. To "discover the secret of life" he started shearing off the legs of toads copulating. But his contributions to science came from other fields.
The majority of the "natural philosophers" of the time, including the great French naturalist Buffon, believed that all small animals such as insects, frogs and mice were born spontaneously, springing from cow dung or mud. Spallanzani was the first to prove that not even a microbe comes from nothing. Observing a single germ under the microscope, he saw it narrow in the middle, then divide, and multiply. Through a long series of experiments he demonstrated that by heating a liquid all the germs in it die and no new germs can generate so long as the container remains. To achieve this he fused the neck of his bottles over a flame.
The implications of this discovery were far too momentous to be realized at once by anyone, including Spallanzani himself, alone to be put forthwith to any practical use. In fact they contained all the notions for the future works of Pasteur and Koch, and for the canning of food for conservation, which could have enabled Napoleon to win his Russian campaign and change the course of history.
With the death of Spallanzani in 1799 we reach the threshold of another century, of a new period for mankind. The world had rid itself of the superstitions of Galenism, except one - which, like the germ observed by Spallanzani had already started dividing and multiplying, taking up ever more monstrous forms.But as yet nobody seemed to have noticed.
THE GREAT ADVANCES IN MODERN MEDICINE
Before leaving definitely the moribund 18th Century, let us briefly see what other important advances were made inside that span, beyond those of Leeuwenhoek and Spallanzi.
Nutrition & Diet eg. Scurvy and Vitamin C
In 1757, when scurvy was decimating the crews of the British Navy to the point of endangering the efficiency of the Home Fleet, James Lind, a doctor of the naval hospital at Portsmouth, advised the Admiralty to add lime juice to the diet of the crews that had to spend many months at sea. Ever since the 16th Century lime juice had been regularly supplied to the Dutch trading ships sailing to the East Indies, and their crews were free of scurvy, and later on the British Merchant ships had also employed lime juice with success. But the Admiralty brains didn't believe that such a simple and inexpensive remedy could cure or prevent such a deadly malady. And yet Captain Cook had followed Lind's advice and remained at sea 3 years without a single case of scurvy developing on board his ship. But it was only after Sir Gilbert Blane cured an outbreak of scurvy in 1784 that the Admiralty gave serious thought to the matter, and in 1795 an order was at last promulgated providing for the issue of lime juice to the crews of the Royal Navy; that is why the English sailors, and later all the Britishers, were called limeys.
Lime juice contains Vitamin C, a potent antidote against scurvy, and this had not been through animals, for a great many of which lime is fatal. Vivisectors later on caused mortal scurvy in innumerable animals by feeding them unnatural diets, and continue doing so today just to prove and reprove what the Dutch of the 16th Century knew already.
Diagnostics: Percussions and Auscultation
Viennese clinician Leopold Auenbrugger had introduced in 1791 the diagnostic method of percussion, consisting of tapping the surface of the patient's chest and abdomen to find out the condition of the parts beneath by the sound emitted. It can reveal the enlargement of the liver or the heart, or an edema of the lung, and it was the forerunner of auscultation, equally important today in diagnostics.
Heart Disease & Digitalis
The first great step towards the cure of heart disease - and so far also the last - was the discovery of digitalis in 1785 by William Whithering, an English physician and botanist. He tested an infusion made of the dried leaves of the foxglove flower - which had been used among the country folk as a remedy for dropsy or edema - on his heart patients, and with such success that it was soon included in the Edinburgh Pharmacoepia. It was named digitalis because the petal of the foxglove flower is shaped like a finger.
Digitalis is among the few drugs in the world's pharmacopia that has proved of lasting value, and it was discovered, like all the other fundamental drugs, without animal experimentation. There is no more valuable remedy today for lowering ventricular rate in cases of a heart disorder now called auricular fibrilation.
Asepsis, Antiseptic Surgery & Iodine
Iodine, another fundamental medicament of lasting value, has been in use as a dressing for some 150 years. That means before the enunciation of the germ theory of disease, and therefore before the nature of infection was propounded by medical science, which during the centuries of Galenism had derided the hygienic precepts of antiquity, confirming that by dint of new wisdom man forgets the old.
In Watson Cheyne's classical Antiseptic Surgery (1882), the first standard use in English on the use of antiseptics, it is recorded that the application of iodine as a dressing for wounds was well known in 1859. The authority quoted is French surgeon Louis Velpeau (1795-1867), who claimed in that year that the practise had already been well established for at least 30 years. This takes us back to 1829, 18 years after the element itself had been first isolated in a pure state by Bernard Courtois.
Quinine and Malaria
In South America the natives used quinine against "swamp fever" (malaria), and with the help of that natural remedy the disease was controlled in Europe, too. Long before that, some thinking individuals had observed that malaria occurs most frequently in the vicinity of wamps, and for that reason many swamps were ordered drained; that was long before anyone had discovered that malaria is transmitted by mosquitoes, and that mosquitoes breed in swamps.
Vaccination & Innoculation
The first "modern" type of vaccination was due to Edward Jenner, who in 1796 inoculated a boy with a smallpox vaccine he had developed. This case is among the best known in medical history, so we need not dwell on it, except to reall that Jenner reached his conclusion after 21 years of clinical observations and reflection, in what we would call today "clinical observation."
Although Jenner had anticipated Pasteur by 80 years, his innovation was by no means the first in history. Vaccination had been practiced in the Orient ever since ancient times, and the Oriental smallpox vaccination had been practied in England for the first time in 1717, when it was introduced by Lady Mary Wortley Montagu, the wife of the British ambassador at Constantinople.
The Turkish method consisted of taking from the pustule of an infected individual as much liquid as had place on a pinpoint and scratching with it the skin of the person to be vaccinated. Sometimes this vaccination ended, like today, in death, so various methods had been devised to decrease the virulence of the liquid: it was left to macerate in water for several days, or else a crust was left in water before it was used. The Chinese blew pulverized crusts into the nose of the people to be vaccinated.
The social position of Lady Mary brought the Turkish method to the British Royal Family, who had a dread fear of smallpox after the young and beautiful Queen Mary had died of it at the end of the previous century. But to play it safe, the king first had the vaccine tried out on six prisoners who were waiting for execution in the Newgate prison.
(For more on this topic see the article The Decline of Smallpox in Great Britain - Vaccination in Doubt. It includes a critique of Edward Jenner's book and theories.)
Thus animal experimentation had nothing to do with the discovery and development of vaccination either, nor could it have had, since the gravest human infections are not transmissable to animals, or take up different forms in them. Later on, to produce vaccines on a large and lucrative scale, the industry took recourse to animals, because medical thought had already been channeled into the one-way direction of animal use; and with what dire results, we shall see. When later it became necessary to develop safer means than on animal tissues, the means were found. Thus once more the use of animals had only retarded medical science and caused untold havoc among mankind.
But before going into this we must see how surgery was freed of the two main shackles that had not only caused it to stagnate in a Galenic condition, but had thrown it back to a prehistoric level.
Surgery: Rediscovery of Methods, Anaesthesia, Hygiene & Asepsis
While in most other fields of science and technology the western world was rapidly making important discoveries, in one field all knowledge was morassed: surgery. Worse, the kind of surgery in the Middle Ages and up to the first half of the 19th Century represented a gigantic step backward compared to the variety of delicate operations that had been performed thousands of years earlier in India, Egypt, and Babylon, then also in Greece and in Rome.
The surgeons of antiquity must have known highly sophisticated techniques, but they had been lost, like the architectural techniques of the ancient Egyptian, Roman and South American cultures. We don't know how some of the ancient surgical instruments that have been preserved were used. But we know that already before Hippocrates' time, hygiene played a basic role in surgical technology no less than in medical art. The Hindu surgeons were instructed to wash their hands and nails very carefully, and never to open their mouths during an operation, lest the wound get infected.
It was probably the Hindu medical schools of the two Hindus, Atreya and Sursuta, at some time of the B.C., that influenced Greek anatomical knowledge and medicine. 6th Century Sursuta's work, one of the greatest of its kind in Sanskrit literature, was especially important for surgery. He described operations, advocated dissection of cadavers for surgical training, and the sterilizing of wounds by fumigation. One can truly say that modern surgical progress has consisted in regressing - in finding its way back at last to what was known thousands of years ago, but had meanwhile been forgotten.
The historians have declared themselves unable to explain why the art of antiquity fell into oblivion, but the reason is clear. The reason was the same that brought about the medieval pestilences: As hygiene was derided as superstition, fatal postoperative infections became so frequent that all major surgery was gradually abandoned, except the inevitable cases of accidents or battle. Also the art of ligaturing blood vessels was lost, to be replaced with the easier and speedier cauterization by means of hot oil or iron. This probably happened during the great wars of the Middle Ages.
What we know for sure is that up to the middle of the past century any advance in the field of surgery was impeded by
1) the fear of pain, and
2) the fear of postoperative mortality from infection, which was very high even in simple operations.
In the surgeon's hands the patients had to go through such tortures that some preferred committing suicide than submit to an operation. The few who were brave or foolish enough to accept, cried and struggled on the operating table, some to the point of insanity, or collapse and death. So the surgeons were valued according to their speed. The record for an excision of a gallstone was supposed to
have been 54 seconds. Guilliaume Dupuytren, who operated up to 1835 and was France's highest-paid surgeon because he was the quickest, used to say that pain can kill like a hemorrhage.
Since human beings, however indifferent to the sufferings of others, are unwilling to face their own, much less to pass on to a better life, the surgeons of the last century had plenty of free time. Most surgery was practised by barbers, and was limited to setting fractured bones, excising external tumors, and performing only inevitable amputations, which often ended in death due to infection.
The rediscovery in France of the knowledge of ligaturing of the vessels by Ambroise Pare - not a medical man, as is generally reported, but a barber - had reduced fatal hemorrhages, but death caused by "blood poisoning" or infection had increased correspondingly. Today we know why.
Cauterization, which in the Middle Ages had replaced ligatures, had had the power to disinfect the wound. But the surgeons didn't realize that, as the germ theory had not been announced, nor had the importance of cleanliness been rediscovered as yet. To protect their long frocks, the surgeons of the time wore over them old overcoats which were never cleaned, for the crusts of blood and pus on them testified to wearer's experience: the thicker the crust the higher the fee.
The two big barriers of pain and infection started coming down almost simultaneously toward the middle of the last century.
Anaesthesia: Conquering Pain
Why it took so long for anesthesia to come into general use in the western worlds is inexplicable, since the pain-killing power of certain plants, like opium and hashish, was already known in ancient times and among primitive people. The oriental doctors of antiquity must have used some sort of anesthesia for their various operations of high surgery. Only Chinese acupuncture has been preserved to our day, and in expert hands its great utility for anesthesia has been proved beyond doubt even to modern science.
In the 13th Century, Michel Scot (Scotus), the Scottish astrologer and alchemist, who translated medical works from the Arabic, wrote for the surgeon a recipe for an analgesic composed of mandrake, opium and henbane; but perhaps no one dared use it because Scot was also a magician, which is why Dante assigned him a place in hell: "Michele Scotto fu, che veramente della magiche frodi seppe il gioco." (Inferno, XX, 116-117)
Three centuries later, Paracelcus imported from the East another opiate, laudanum, and among his recipes found after his death there was one he had called "sweet vitriol", which on examination turns out to be today's ether. In fact, the Middle Ages was the period of the various sleeping potions; the literary works, including Shakepeare's, are full of references to drugs that induced deep, death-like sleep.
The first modern anesthetics were found by chance - it couldn't have been otherwise - and by personal experience. As early as 1800 Sir Humphry Davis suggested that nitrous oxide might serve the purpose, and in 1803 the German pharmacist Friedrich Serturner had derived morphine from opium; but probably because he had tried it on dogs, in which morphine can cause maniacal excitement, its value as an anesthetic was not recognized for several decades.
Horace Wills, an American dentist, finally used Humphry Davy's nitrous oxide to extract the tooth of a colleague, and thus the so-called laughing gas found its way into practice. Then in 1846 Dr. William Morris, an American dentist functioning as the first anesthetist, enabled John Collins Warren to perform the first surgical operation under ether anesthesia at the Massachusetts General Hospital, in front of numerous students and doctors. It was a complete success. The fight against pain was won.
The next year James Simpson - after tests made on himself and on friends - used chloroform (known since 1828) for the first time in a surgical operation. But scientific information being less fluent and widespread in the last century than today, in France Flourens decided some years later to experiment with chloroform on animals, and the results led him to discard it as an anesthetic altogether, while in England Sir Lauder Brunton's experiments on 490 dogs, horses, monkeys, goats, cats and rabbits, under the auspices of the Hyderabad commission gave results which were ridiculed by all the leading British anesthetists. (Lancet, Feb.8, 15, 22, 1890)
So once more, animal experiments retarded the adoption of one of the most useful drugs of all times.
The inventor of lumbar anaesthesia was German doctor August Bier, who had himself injected with a 1% solution of cocaine into his spine in order to observe its effect. Sigerist, the historian, states in his already-mentioned work: "Bier in 1899 announces the immortal lumbar anesthesia, the invention that brings his name into the history of medicine."
As the second British Royal Commission Report on Vivisection was officially to establish: "The discovery of anaesthetics owes nothing to experiments on animals." (p.26)
Rediscovery of Surgical Hygiene & Asepsis: Semmelweis
But meanwhile medical art had already effected the greatest progress of all by starting to return to the long-forgotten hygienic principles. The year 1847 had marked the beginning of the war on infection, thanks to Philip Ignaz Semmelweis, a Hungarian who was director of Vienna's Allgemeines Krankenhaus (General Hospital). In that city hospital, puerperal fever was killing one childbearing woman out of four - the same rate of mortality as occurred at Massachusetts General Hospital in cases of amputation. In Paris the situation was even worse: 59% of the amputees used to die. Abdominal operations were rarely tried before the discovery of anesthesia, and if they were tried, the results were even worse. In England 86% of the women subjected to Caesarean section died.
Semmelweis hadn't seen a germ any more than Hippocrates ever had, nor had he heard anything about a germ theory, which was still to be announced; but both physicians had reached the same conclusion thanks to true medical intuition and the sheer exercise of their intellectual powers - the intelligent clinical observation that had solved so many great medical problems.
Others before Semmelweis had suggested that puerperal fever might be a contagious disease, and that hygiene could prevent it; but they had been laughed at. Animals didn't get sick and die of fever when they gave birth; so why should people.
In 1795 Scotsman Alexander Gordon gave ample proof that the disease was contagious, in a paper titled Treatise on the Epidemic Puerperal Fever of Aberdeen, in which he stressed the need for disinfection of doctors and nurses attending lying-in women. Although the evidence he offered was indisputable, it went under amid the general hilarity of the medical giants of the time.
In 1843 Oliver Wendell Holmes, professor of anatomy and physiology at Harvard, and father of the namesake jurist, wrote The Contagiousness of Puerperal Fever. It also met vigorous opposition from the leading obstetricians, and its facts began being acknowledged only after it had been enlarged and re-printed in 1855. The late English historian, Lord Moynihan, called it "one of the greatest essays ever written in the history of medicine." Semmelweis had not heard of the English works when he came to the same conclusion and put them into practice.
It happened the day Semmelweis interrogated a lying-in patient who was in despair because she had been assigned to the ward of the obstetrics students rather than to the midwives. From her, Semmelweis learned that the women of Vienna were convinced that with the students they risked death much more then with the midwives. At that moment Semmelweis had his flash of intuition that started modern medicine toward its most important conquest - the restoration of pre-Galenic hygiene, long before Pasteur came along.
A few days earlier Semmelweis had seen a colleague die, who had cut and infected himself while performing an autopsy on a victim of puerperal fever, and had shown the same symptoms as the women who died of puerperal fever. The students also performed autopsies; not the midwives. So Semmelweis concluded that puerperal fever must be of infectious nature. For this reason, and not because they were less able, more students than midwives infected the lying-in patients.
That very day Semmelweis began his war against contagion: He demanded absolute cleanliness and disinfection by chlorination, of everybody connected with the maternity ward. But the doctors didn't like this innovation which they considered humiliating and ridiculous. However, within a couple of years, Semmelweis reduced mortality in the maternity ward by 90%. But he got no credit for it, because he couldn't demonstrate his theory through an animal experiment, which were already the great vogue. And when he started calling assassins the obstetricians who still refused to wash their hands, the Austrian doctors banded together and had him ousted.
Semmelweis returned to his native Budapest and published a book about his findings. But as his countrymen also derided him, he became insane, and he died without seeing the triumph of his ideas.
Semmelweis and the few of a like mind obtained recognition a quarter of a century later, when the germ theory was announced - another fundamental step that owed nothing to animal experimentation.
Thus the other great danger of surgery was eliminated - post-operative infection.
As soon as the two great barriers that stood in the way to surgical progress - infection and the fear of pain - were removed, surgery developed rapidly, as operations became possible that had never been tried in modern times, and the surgeons, first exploring dead bodies, then operating on the living, perfected within a few years the techniques that are fundamentally still in use today.
For over a century the vivisectors had done surgical exercises on animals, without having to worry that the pains they were inflicting or the danger of infection, but surgery had been unable to rise above the medieval morass. It was only when it became possible, thanks to anesthesia and asepsis, to operate directly on man that surgery recouped in a few decades practically everything that had been lost in the Dark Ages.
And soon another discovery that had nothing to do with animal experimentation came to the surgeons' aid, revealing to them beforehand exactly where to cut: Roentgen's X-rays.
Surgical Training
"Practice on dogs probably does make a good veterinarian, if that's the kind of practitioner you want for your family."
So wrote Dr. William Held, internationally famous Chicago physician - one of the many great medical men who regarded the practice of vivisection as dangerously misleading for medical art.
It is not hard to understand why exercises on dogs - the favorite animal of the surgical experimentor - can't develop surgical skill in respect to human patients. In the dog's narrow, peaked chest the operational field is so different from man's that operations require in part specially built instruments. Also the shape and disposition of all organs differ markedly. So the surgeon who has learned to locate, say, the femoral artery in the dog, will find it hard afterwards to locate it in a human patient. And the skin, tissues, tendons, in sum all parts of the dog, react differently under the knife, being either more elastic or tougher or less so than in man. The postoperative reactions also differ. So all animals are much less subject to infections, and the surgeon who has succeeded in cutting up a dog without killing it credits his own skill rather than the animal's greater resistance: a dangerous illusion.
Likewise the vivisectionists' claim that our knowledge of human heart surgery derives from exercises on dogs is plainly absurd; since the dog has a highly irregular, intermittent pulsation, there couldn't be an unsafer guide to man's heart.
All our knowledge of the human heart derives from the section of cadavers, from accidents in which the doctors had to intervene directly on man to save his life as in the countless cases of battle injuries and traffic accidents - and through radiological observations. Obviously, those practicing surgeons who happen to be fond of vivisection will claim that they derive their skill through "working" on animals. My advice to those in need of surgery is to keep away from such people, since they are dangerous surgeons and pitiless men.
The same holds true for brain surgery. The millions of animal experiments that purported to ascertain the localization of the cerebral functions have merely created confusion, adding nothing useful to the teachings of Hughling Jackson, who had never experimented on an animal. And this had been clearly predicted by Jean-Martin Charcot (1825-1893), the father of modern neurology: "Experiments on animals designed to establish the localization of the cerebral functions can teach us at best the topography of that particular species - never the topography of man." said Charcot. Even Claude Bernard had realized that.
Now let us take an x-ray look at the vivisectionist's battle-horse: the blue babies case.
Blue Babies
"Blue babies" defines newborns suffering from a defect to the pulmonary artery that carries venous blood to the lung. Because the oxygenation of the blood is insufficient in such children, their skin appears bluish and they develop shortness of breath. They seldom survive to maturity if left untreated.
To remedy that condition, American surgeon Alfred Blalock had introduced in 1944 an operative technique based on clinical observations [of humans] made by heart specialist Helen B.Taussig. Blalock claimed to have developed his technique through numerous excercises on dogs - however puzzling such a statement may sound to anyone who is unaware of the anatomical, organic and functional differences between the heart of man and dog.
Then the London surgeon R.C. Brock of Guy's Hospital developed an entirely different technique by careful postmortem observation [of humans] correlated with symptoms evinced during life, and the application of sound reasoning. The report in the British Medical Journal (June 12, 1948) makes it quite clear that the
whole procedure was evolved without experiments on animals at any stage.
A third technique, not involving animals either, was developed by two English surgeons, N. R. Barrett and Raymond Daley of St. Thomas Hospital, London. This technique was developed along the lines of logical deduction, as described in the British Medical Journal (Apr.23, 1949).
The survival rate in all these cases is the same, proving once again - if further proof were needed - that those who try out something on animals - do so not because they have to, but because they want to - like that enthusiastic vivisector Alfred Blalock, inventor of the "Blalock Press" designed to crush without effort the extremities of dogs.
The British surgeon-historian M. Beddow Bayly had this comment in his Clinical Medical Discoveries (1961): "It is significant that both of the latter methods have proved of value in cases that are unsuitable for the treatment by Blalock's method ...Finally, there is no reason to believe that Blalock's operation, based as it was on logical reasoning, just like Brock's, could not have been applied with as much success to human patients without the preliminary recourse to practice upon dogs. If this was unnecessary to Brock's success in this country, it is surely logical to conclude that it was equally unnecessary in the United States."
In Great Britain surgeons have had for a century experience with human patients only, for under the Cruelty to Animals Act of 1876 it is provided that no experiment shall be performed on animals for the purpose of attaining manual skill. And it would be very difficult for anyone even today to disclaim Heneage Ogilvie, medical doctor and Consulting Surgeon to Guy's Hospital and Royal Masonic Hospital, who declared in the British Medical Journal (Dec. 18, 1954, p.1438):
'British surgery has always stood high because it can be claimed, and not without reason, that every surgical advance of major importance have come from this country."
But even more revealing is what the vivisectors themselves say in their unguarded moments about the uselessness of vivisection for medical science. In Experimental Surgery, the monumental vivisection manual (Baltimore, 1949) J. Markowitz gives fair warning in his introduction that "The operative technique described in these pages is suitable for animals, usually dogs. However, it does not follow that it is equally and always suited for human beings. We refuse to allow the student the pretense that what he is doing is operating on a patient for the cure of an ailment."
So this top expert states explicitly that vivisection doesn't really help train the surgeon, he even says it can be misleading, and furnishes a memorable example: "In our student days intrathoracic surgery sounded very mysterious and formidable. We know today that it need not be so. What caused the difficulties was that the surgeons assumed the nature of pneumothorax as encountered in the dog to be similar to what will occur in man. This is only true for the side that is opened, for a man has two separate chests, each harbouring a lung, and each capable of sustaining life... In the dog, even a small puncture of one pleural cavity will cause fatal collapse of both lungs."
(Here we shall skip pages 172 to 180 of Hans Ruesch's book until we have time to upload it to this page. That section contains content and quotes from eminent scientists, the type of which can be found on this page about the progress of surgery and surgical training.)
Germ Theory, Vaccines & Other Confusions
Only to leave none of the vivisectionist claims unanswered: For the experiments of Galvani and Volta - which didn't concern medicine in the first place, but electricity - no living frog was used, but a dead one. "The metallic couple excites in the dead frog the nerve that directs muscular contraction." (Enciclopedia Italiana: "Galvani"). Volta soon renounced working on dead frogs, having found more suitable experimental material in inorganic matters. (Op. cit. "Volta")
The incredible confusion reigning today in medicine extends to the historical and school texts. So the Encyclopedia Americana (ed. 1972) states that Sir Charles Bell discovered in 1807 that the anterior spinal nerve roots are sensory (Bell's law), and under Magendie's law: "demonstrated what is known as Magendie's law: that the anterior spinal nerve roots are motor in function and the posterior are sensory." A historical examination of the two men's recorded conferences and writings prove that Magendie tried to usurp the Scotsman's discovery, having brought no contribution whatever to physiology, in spite of his innumerable vivisections.
Compounding the confusion, the Britannica claims that Galen already discovered practically as much almost 2,000 years ago: "He performed sections of the spinal chord at various levels and observed the resulting sensory and motor disturbances and incontinence."
But in the column "Science" of that very same encyclopedia, one is surprised to learn that some other scholar attributed that same discovery to a whole school: "At Alexandria the teachers' experiments on animals led them to distinguish between the posterior nerve roots of the spinal cord, which convey sensation, and the anterior, which convey the motor impulses."
Germ Theory
As for Pasteur, most encyclopedias, including the Britannica and the Americana, credit him with the discovery that germs don't spring into life spontaneously, but originate from other germs, and that heat kills them. It was in fact Spallanzani who demonstrated this a whole century earlier.
Spallanzani's were the principal steps taken in bacteriology, after Leenwenhoek's discovery of the existence of the germs. Pasteur carried Spallanzani's experiments a step further, determining exactly how high the temperature had to be, and how long the exposure to heat, before the germs were dead.
Antoine Bechamp (1816-1895), Doctor of Medicine and of Science, professor of biochemistry and physics and lecturer at the University of Paris, preceded Pasteur in his development of the germ theory. Contrarily to Pasteur, Bechamp was a humane researcher, and it is interesting to note that as in the controversies between Bell and Magendie, between Tait and Lister (asepsis and antisepsis), between Pasteur and Bechamp and between Koch and Bechamp, time proved the humane researchers right.
For Pasteur and Koch a germ was a disease, and a disease was a germ. Today we know that the germ does not necessarily cause the disease, and the disease can insurge without the presence of that particular germ.
Bechamp was among the forerunners who attached more importance to the "soil" (the body) than to the "seed" (the germ). Furthermore, official records show that in regard to many discoveries with which Pasteur was credited, such as that of the origin of silk-worm diseases, Bechamp had been first.
In fact Pasteur profited like few scientists from the discoveries of others. The Dutchman Leeuwenhoek had first seen a germ, Italy's Spallanzani had shown that germs can only come from other germs and that heat kills them, Frenchman Cagmard de Ia Tour had known ever since 1837 that the fermentation of beer is caused by germs that he had identified. Germany's Schwamm had published a paper demonstrating that meat rots only following an invasion of germs, but in 1864 Pasteur arrogated for himself the merit of all these works by presenting a "germ theory", without even mentioning his trailblazers; and he was so convincing that London's great surgeon Lister wrote him a latter of thanks, and today's encyclopedias continue attributing to Pasteur exclusively what by right belongs to others.
Robert Koch was the first to obtain a pure culture of anthrax germs responsible for the cattle and sheep disease, and Pasteur made a vaccine from it by reducing the power of the germs. Many historians call that the first vaccine in history, as if Jenner and the Orientals had never existed. At any rate, an immediate controversy between Pasteur and Koch ensued, each one accusing the other of plagiarism.
Rabies vaccine
Pasteur then proceeded to develop a vaccine against rabies, or hydrophobia, which may represent the most disconcerting case in the entire disconcerting field of vaccines.
Only an infinitesimal percentage of people bitten by a rabid animal catch the infection. But if it develops, it is supposed to be always mortal. So to be safe, everybody who has been bitten by an animal suspected to be rabid gets the special treatment developed originally by Pasteur. But sometimes the vaccinated person dies anyway. In that case the death is attributed to a defective vaccine. But often it has been demonstrated that the vaccine and not the bite caused the infection - for instance when the animal later on turned out to be healthy. Even if the animal is rabid, the bite seldom causes the infection - and never causes it if the normal hygienic rules are followed, like the immediate washing out of the wound with water.
In his best-selling Microbe Hunters, (Harcourt, Brace, 1926/1953) Paul de Kruif gave a highly fanciful account of 19 Russian peasants who, bitten by an allegedly rabid wolf, traveled to Paris in order to receive the newly announced Pasteur treatment from the old master himself. According to de Kruif, 16 of these Russian patients were "saved" by Pasteur's shots and "only three" died. Pasteur became an international hero after that exploit and contributed substantially to the glamorization of "modern" laboratory science. Three deaths out of 19 makes over 15 percent casualties. But knowing, as we know today, that not one in a hundred people bitten by a rabid dog is likely to catch the infection, we must infer that at least some and probably all three of those Russian peasants died because of Pasteur's vaccine, as did uncounted people later on. Besides, at the time there were no facilities in Russia to find out whether a wolf had rabies. Hungry wolves attacking villagers in winter were a common occurrence; and even today many people, in Italy for instance, believe that any dog that bites them must be affected with rabies, otherwise it wouldn't have bitten them.
Some informed doctors believe that rabies, as a separate and distinguishable disease, exists only in animals and not in man, and that what is diagnosed as rabies is often tetanus (lockjaw), which has similar symptoms. Contamination of any kind of wound will cause tetanus, and it is interesting to note that today in Germany those who get bitten by a dog are regularly given just an anti-tetanus shot. According to Germany's most authoritative weekly, exactly 5 Germans are supposed to have died of rabies in 20 years (Der Spiegel, 18/1972, p.175). But how can anyone be sure that they died of rabies? Hundreds die of tetanus.
Among the many doctors I have questioned in the US and Europe, I have not yet found one who can guarantee that he has seen a case of rabies in man. The number of cases reported by the U.S. Public Service in its Morbidity and Mortality Annual Supplement of 1970 was exactly two --- among 205,000,000 people. Provided the diagnosis was correct.
This compares with 148 cases of tetanus reported, 22,096 of salmonellosis, 56,797 of infectious hepatitis, 433,405 of streptococcal infections and scarlet fever.
Doctors who are faced for the first time with a case of suspected rabies complain that they have no precedents to go by. The main difficulty Pasteur met with in perfecting his alleged vaccine, which often caused paralysis, consisted in finding rabid dogs; finally he had to get healthy dogs, open their cranium and infect them with the brain substance of the only rabid dog he had been able to get hold of.
Pasteur never identified the rabies virus. Today, everything concerning this malady is still more insecure than at Pasteur's time.
Only one thing is sure: ever since Pasteur developed his vaccine, the cases of death from rabies have increased, not diminished.
Currently, rabies is presumed to be established in autopsies by the presence of 'Negri corpuscles', so named after an Italian physician who in 1903 declared to have discovered them in the plasma of the nerve cells and the spinal nerves of rabid dogs. However, Dr. John A. McLaughlin, a prominent American veterinarian who in the sixties was called to investigate a widespread outbreak of alleged rabies in the State of Rhode Island and performed numerous autopsies on dogs during the height of the scare, found animals with "rabies" symptoms that had no Negri corpuscles whatever, whereas dogs that died of unrelated diseases had them in abundance. A veterinarian from Naples, where there is a fixation of fear of rabies, showed me in a textbook the image of a Negri corpuscle - the only one he had ever seen - it looked indistinguishable from the Linz-Sinigallia corpuscles that occur in dogs who have distemper. Nobody knows how many dogs affected by mere distemper have been killed by order of sanitary authorities whose zeal overshadowed their knowledge.
A few years ago, Dr. Charles W. Dulles, widely-known Philadelphia physician and surgeon and lecturer at the University of Pennslyvania on the History of Medicine, had this to say: "I might cite my own experience in the treatment of persons bitten by dogs supposed to be rabid, which has furnished not a single case of the developed disease in 30 years, and I probably have seen more cases of so-called hydrophobia than any other medical man."
Every real expert is aware that nothing is known for sure except what Hippocrates already knew: that the best protection also against this infection is cleanliness. The No.523 of the World Health Organization Technical Report Series, entitled WHO Expert Committee on Rabies, Sixth Report, 1973 (meaning that there have been no less than five previous WHO reports on the same subject) announces that evidence is accumulating that parenteral injection of anti-rabies vaccine causes human deaths "under certain conditions" (p.20), and states (p.17): "The Committee recommends that production of Fermi-type vaccines, since they contain residual living virus, should be discontinued."
"Residual living virus" is a pretty serious charge to bring from high quarters against a vaccine, but nobody seems to pay much attention to all this, or to understand what it means. It simply means that probably the very rare cases of humans who died of what has been diagnosed as rabies, have not died from something received from a dog but from a doctor.
But the climax of that WHO report is on page 27: "The Committee emphasized that the most valuable procedure in post-exposure treatment is the local treatment of wounds. This should be done by thorough washing with soap and water..." And on the next page the point is repeated: "Immediate first-aid procedures recommended are the flushing and washing of the wound with soap and water." So it took no less than 6 reports by WHO "experts,' to reach the conclusion that Hippocrates had been advocating.
In fact whoever reads carefully this and other WHO reports, notices that serious students of medicine can can rely on very little except Hippocratic hygiene and common sense. But WHO can't admit it, otherwise the public might ask: "What is the use of WHO?" WHO is housed on one of the biggest, costliest buildings of modern times, with large, empty halls, libraries lined with every medical publication issued throughout the world, with numerous executives who draw fat salaries to do nothing and a regiment of smart secretaries to help them. This huge real estate complex, surrounded by the silence of well-groomed lawns and flower gardens is one of the most beautiful Alpine settings outside Geneva, represents the counterpart of the millions of laboratory animals wasting away under scientific torture the world over.
Lately, still a new vaccine against rabies has been developed, which has been described as a "fantastic breakthrough" by WHO officials. The report in Time (Dec.27, 1976) reads in part: "Writing in the Journal of the American Medical Association, a team of US and Iranian doctors last week reported that they recently administered the vaccine in a series of only six shots to 45 Iranians who had been bitten by rabid animals. Not a single victim developed rabies, or showed a severe allergic reaction. Reason: the new vaccine, unlike the old, is cultured in human rather than animal cells. Thus, while the patients develop antibodies against rabies, they do not suffer fatal reactions to the foreign animal protein."
For the past hundred years anti-vivisectionists and other sensible people have been saying that there must be better ways for medical science than the ones recommended by Claude Bernard, and that Pasteur's alleged anti-rabies vaccination was humbug. Now official science is at last catching up to this obvious truth, and all the big men want to get into the act.
A headline in Germany's medical news weekly Selecta (May 16, 1977), which read "Problem of Rabies Vaccine Solved?" must have surprised many readers who had until then been led into believing that Pasteur had solved that problem long ago since it has always been presented as his main claim to fame. The article reported a round-table of German virologists who gave hell to Pasteur's alleged vaccine and cited one Prof. Richard Haas who had defined it "an archaic monster."
The Giants with Feet of Clay
Compared to histrionic, ebullient Pasteur, Koch was a quiet individual. Like Pasteur, Koch also rendered himself useful at the microscope, whereas all his attempts to parallel man and animal were failures that retarded or tragically misled medical research. Nonetheless, Pasteur and Koch are still being presented in the textbooks as the medical giants of our age.
In fact, it was through trusting in animal experimentation that Koch made one of the biggest blunders of his time - one which revealed itself as a blunder only years later, after Koch had received the Nobel Prize for it, and after it had caused the death of innumerable people.
Tuberculosis & the Tuberkulin Disaster.
Toward the end of the last century, in the great industrial cities of the north, one person out of seven died of tuberculosis, or TB for short, and usually in youth. Koch's announcement in 1882 that he had discovered and isolated the specific germ was greeted with an explosion of joy the world over. At that early stage of the game nobody had noticed that in animal tissues in which human tuberculosis could propagate, the disease took on quite different forms.
The discovery of the tubercle bacillus seemed to sweep away all the other causes for TB that had been advanced: surroundings, air, diet, and the individual physical or psychic disposition, also called the soil. The world had reached the unshakable conviction that medicine had really become an exact science, and that the Six Postulates first enunciated by Koch's teacher Jakob Henle in 1840, later renamed the Six Postulates of Koch, had been proved right.
Those Postulates may be summed up thus:
- 1. A specific causative organism (Erreger) should be found in all cases of an infectious disease.
- 2. This organism should not be found in other diseases.
- 3. It should be isolated.
- 4. It should be obtained in pure culture.
- 5. When inoculated to animals, it should reproduce the same disease in them.
- 6. It should be recoverable from the experimental animal.
Says the Encyclopedia Britannica still in our days:
"Every modern student of bacteriology learns Koch's postulates as part of his basic training."
Contemporary teachers of medical history report in all seriousness as absolute fact what has long ago been debunked.
Today we know the utter nonsense of such claims; but the textbooks have given up trying to correct all the mistakes that keep surfacing, and let them ride even in the new editions.
We know today that the "specific organism" (or germ) causing a disease in man never reproduces the identical disease in animals: animals can't be infected with our cholera, typhoid, yellow fever, leprosy, smallpox, bubonic plague, our various flu's, etc. Not even with our common cold. Koch's contemporaries and the "scientists" who recommended him for the Nobel Prize didn't know that yet.
The universal belief before the end of the last century was this: Since every disease is caused by a specific germ, all we have to do is to identify this germ, culture it, infect animals with it, recover it from the diseased animals, obtain a vaccine, and inoculate humanity with it. This had become - for a while - a dogma of the official science, and whoever expressed doubts was a heretic, a regressive fool. No one was allowed to doubt that all the diseases of mankind would be definitely eliminated before the end of the century, which was still 18 years away.
Probably nobody doubted Pasteur when he proclaimed in his emotional voice and flowery style: "If the conquests useful to mankind move your heart, if you are amazed at the effects of electric telegraphy and so many other admirable discoveries, then you should take interest in those sacred sites that are called laboratories... They are the temples of the future, of riches and welfare... That's where humanity becomes better..."
Even while Pasteur was uttering these idealistic words, humanity for the first time in its history was beginning to contract mortal diseases, fabricated in laboratories through animal tortures with great effort and at high cost. Eight years after identifying the TB bacillus, Koch had announced to an ecstatic world that he had perfected a vaccine he had named Tuberkulin, which miraculously cured "tuberculous" guinea-pigs. And in the following years, thousands of people rushed to get themselves inoculated with what can aptly be defined the first of the modern "miracle" drugs.
It turned out to work the same kind of miracles that thousands of miracle drugs as yet to come were to achieve: it worked financial miracles for its manufacturers and the medical profession, including Robert Koch, who in 1905 got the Nobel Prize for it; but it spelled disaster for the credulous public. Many years had to pass before the new medicine men had to admit that Tuberkulin cured tuberculous guinea-pigs only. Instead of protecting human patients from catching TB, it proved capable of causing it in human patients, and it invariably activated latent forms of the malady. Tuberkulin has not only long since been discontinued as a vaccine but has even been used as a diagnostic means: The human organism reacts so violently to this drug that it can reveal an individual's predisposition to the infection.
Today we know that TB does indeed depend on the environment, on the air, on the nourishment, on individual physical and mental disposition, as proved by the millions of people who come in daily contact with tuberculous persons without catching the disease and the fact that it is still today four times more frequent among the poor and undernourished than among the well-fed. But meanwhile, in 1901 Koch had already announced to a stunned Congress of Tuberculosis in London that TB is one malady when it occurs in animals and quite another when it occurs in people.
Cholera
Before that, in Alexandria, in 1883, an epidemic of cholera had broken out. Immediately Germany and France dispatched their microbe hunters to seek out and find the responsible agent. The German team was headed by Koch, the French team by two of Pasteur's assistants K.Roux and L.Thuillier, each team working on its own and against the other.
In Alexandria, both teams collected intestinal juices from the cadavers of Alexandrians who had just died of cholera and injected them into dogs, cats, monkeys, and mice. But the animals thrived on those juices. While the microbe hunters were still wondering why, the epidemic, like all epidemics in the past and present faded away as mysteriously as it had come, and the microbe hunters sailed back home. Not all of them: on the morning of departure, Thuillier developed the symptoms of cholera, and before evening he was dead.
Actually Koch had already recovered from the intestines of dead Alexandrians the comma bacillus associated with cholera, but as all cultures of it that he injected into animals caused them no harm, he had ruled out the possibility that it was the responsible agent. Today we also know that the comma bacillus dies at once in any animal.
Koch then persuaded the Kaiser to send him to Calcutta, where among the un-hygienically crowded populations some cholera epidemics were always smoldering, then as now. Again he found the comma baccilus in the intestines of bodies dead of cholera, but not one in any of the healthy Hindus he examined. So he came to the conclusion that, although harmless to animals, the comma bacillus was the responsible agent in man.
Today we know it is not so; that sometimes the comma bacillus cannot be found in individuals dead of alleged cholera, and yet it can be found in people who are well, in the so-called healthy carriers. At any rate, the defeat of cholera, which some people ascribe to the vaccine, others to improved hygiene, was also retarded by Koch's belief in animal experimentation.
Back from India, Koch received a hero's welcome, and from the Kaiser's own hands the Order of the Crown with Star. But at Munich a spoilsport was waiting for him in the person of the old professor of hygiene, Max Pettenkofer, who through the introduction of elaborate sanitary services had made of Munich the healthiest city in Europe, and clung to the belief that not the virulence of the seed but the inadequacy of the soil was responsible for the infection.
"Your bacillus can do nothing, dear Koch!" the old lion roared at our puzzled hero. "What counts is the organism. If your theory were right within 24 hours I should be a dead man." He grabbed from Koch's hand a tube filled with a pure culture of cholera germs, enough to infect a regiment, and in front of his horrified colleagues he swallowed the entire contents.
But only Koch felt sick.
Why does a microbe cause a disease in one organism but not in another? Koch and Pasteur had not yet asked that question - which today still begs an answer - although the vivisectors have tried to extract it with violent means from millions of animals.
That microbes associated with a malady may abound in the environment and be present in the human body without giving rise to symptoms is by now a well-known fact. In 1909 Lancet (Mar 20, p.848) pointed out: "Many organisms which are considered to be causal are frequently to be found in healthy persons. The organisms of enteric fever, of cholera, and of diphtheria, may be cited as examples of this."
It is fantastic to note how once science has decided to give a theory dogmatic validity, it will cling to that theory, all counterproof notwithstanding. The theory of the Six Postulates, although disproven by the experimenters themselves, had been given dogmatic validity. That it has not yet been removed from our textbooks is due perhaps to the recognition that there is no guarantee that any of the other theories which keep cropping up will prove still valid when the next edition is published. Why spend time and money to replace an old bloomer with a new one?
The effectiveness of vaccination is always difficult to determine because in every case case counterproof is lacking. We have no way of knowing whether the decrease of an infection is due to a vaccine or not. For sure we know only what Hippocrates knew: that the most effective and at the same time harmless prevention of contagion is hygiene.
Diseases came and went without any vaccination.
The bubonic plague that caused millions of deaths during the Middle Ages [pretty much] disappeared without any vaccination. Leprosy [pretty much] disappeared from Europe without any specific therapy. The Swiss medical historian Ackerknecht puts it this way: "Leprosy, a rare disease in antiquity, started spreading conspicuously in the 6th Century, reached a terrifying peak in the 13th Century, then vanished mysteriously from Europe." (Op. cit. p.83) Syphilis has lost its erstwhile virulence. Many other infectious diseases underwent mutations in the course of the centuries, to be replaced by new ones.
All this tends to prove that the great diseases of mankind have a life cycle of their own - they spring into being, grow, and decline, all without any discernable reason. As usual, man deludes himself that he is the protagonist on earth; but nature is. Medical science today knows nothing with certainty that Hippocrates didn't know. On the other hand she has forgotten or is neglecting a great many valid notions, by dint of turning out, with unshakeable presumption, new biochemical theories almost daily.
In 1931, an article in the Paris daily, Le Matin, reported: "Once more the census proves that France's decreasing population is not due to any decline in births but to increased death rate . . . The increasing death rate is greatest among infants, the very class that is being subjected to wholesale 'protective' vaccination."
Smallpox Vaccination
Dr. G. Buchwald, the German medical director, whose extensive studies of the effects of smallpox vaccination's leading to encephalitis eventually were determinant in the German government's recent decision to abolish smallpox vaccination altogether, expressed his suspicion in several scientific works that multiple sclerosis also could be a belated consequence of the smallpox vaccination (Der Deutsche Arzt, 1971, VoL 19, p.1007, id., 1912, VoL 3, p.158, and Medizinische Welt, 1972, 23, p.758).
Prof. Rene Dubos had already written in Man, Medicine and Environment (Praeger, New York, 1968, p. 107): "Smallpox vaccine does produce serious encephalitis in a few persons even when administered with the utmost care. The chance of contracting smallpox is now so slight that the risk of accidents originating from the vaccine is much greater than the chance of contracting the disease itself."
And the French magazine Vie et Action (March / April 1966, p.9) had this comment: "In Great Britain, smallpox vaccination hasn't been compulsory since 1898, and yet five times fewer people have died of smallpox in Great Britain than in France, where this vaccination is compulsory. The same goes for Holland. Now Great Britain and Holland are nations that continuously have contact with hundreds of thousands of seafarers from all over the world, notably from countries where smallpox is frequent. And yet abolition of vaccination and the enforcement of the natural hygienic measures have clearly proven sufficient to eliminate smallpox and the so-called infectious maladies."
(For more on this topic see the article The Decline of Smallpox in Great Britain - Vaccination in Doubt. It includes a critique of Edward Jenner's book and theories.)
The powerful American pharmaceutical lobby was able to oppose much longer than the British the abolition of compulsory smallpox vaccination. Up to 1971, the millions of people who every year entered the U.S. had to be vaccinated against smallpox and the vaccination was considered valid only for five years.
As ever more cases of smallpox developed among people vaccinated inside that period, the Washington lobbyists actually succeeded in "persuading" the US. health authorities that vaccination was "effective" for only two years instead of five - ensuring profits and new cases of encephalitis (severe, frequently maiming or deadly inflammation of the brain), and what-have-you among the vaccinated. Unheeded went a few isolated protests like the one by Dr. Charles Henry Kempe, famous medical researcher of Chicago University, who in Philadelphia's Evening Bulletin (May 7, 1965) recommended abolishing smallpox vaccination, stating that since 1948 there had been no deaths from smallpox in the U.S., but in the same period more than 300 had died from smallpox vaccination, including vaccination-induced encephalitis.
A few years later, at last, compulsory vaccination was quietly dropped by the U.S. It could no longer be kept from the public that fewer people had died from smallpox than from the consequences of vaccination. And immediately many countries followed suit.
American vivisectionists tried to explain that vaccination was no longer necessary in the U.S. because the disease had been virtually wiped out by the previous vaccinations. They neglected to remember that each year millions of foreigners including hundreds of thousands of illegal unvaccinated immigrants from Canada, Mexico, Africa, and the Far East - cross the border into the States...
Hygiene: The Decline of the Infectious Diseases
All the medical historians of our century, from Henry Sigerist to Brian Inglis, from Rene Dubois to Beddow Bayly to Ivan Illich, agree that the decline of the epidemics which had wrought havoc in the Middle ages was not due to the introduction of vaccination, but of hygiene, for they had diminished long before large-scale inoculations had begun... but most of today's medical journalists blithely dismiss the major historians and statistical evidence and continue to con the public, stating that the epidemics have been eliminated thanks to vaccination.
The financially profitable aspect of vaccination for the manufacturers is undisputable...
Polio - Salk Vaccine
The discovery of Salk's polio vaccine was greeted with a wave of enthusiasm... But already before Salk developed his vaccine, polio had been constantly regressing...
(Here we are up to page 195 of Ruesch's book ... To be continued ...)
Page 198:
Life Expectancy
Just as the introduction of asepsis, antisepsis, ether, opium, curare, cocaine, morphine, chloroform, and other forms of anaesthesia, all of determinant importance for the rebirth of surgery, owe nothing to vivisection, so the thermometer, microscope, bacteriology, stethoscope, opthalmoscope, X-rays, percussion, auscultation and electronic microscope, all of capital importance for diagnostics, owe nothing to animal experimentation either.
The same applies to the development of vaccination and all the fundamental drugs like digitalis, strophantin, atropine, iodine, quinine, nitro-glycerine, radium, penicillin. Not one single important therapeutic discovery is due to vivisection, whereas books can be filled with the cases where animal experimentation has indisputably spelled disaster for humanity, besides misleading or retarding clinical research."
Some articles regards Hans Ruesch, the author of the above text:
- Wikipedia page about Hans Ruesch
- Article: The World's Most Unsung Hero: Hans Ruesch
- Article: New York Times tribute to Hans Ruesch
- Article: The Man Who Cried "The Empress is Naked!"
Similar Articles:
- This 11-page PDF provides a similar account on the history of modern medicine and decline of mortality from infectious diseases - an excerpt from Dr Robert Sharpe's book "The Cruel Deception" ... The PDF is also available from here.
- Dr. Charles Bell Taylor, M.D. discusses medical advances like: circulation of the blood, electricity, anaesthesia, antisepsis, surgery, glaucoma, functions of the brain, Pasteur, rabies, anthrax, Koch, tuberculosis ...
- Dr. M. Beddow Bayly on medical advances like: stethoscope, radial pulse, blood-pressure, hypodermic syringe, anaesthetics, blood-transfusion, surgical skills, pharmaceutical drugs...
- Why Do Pharmaceutical Drugs Injure & Kill So Many People? Are we the real guinea-pigs? Medical journals report that pharmaceutical drugs kill over 100,000 people and seriously injure millions, each year, in just the USA. Other studies claim the figures are higher. This article explains how drug companies use unscientific tests to make their products look "safe" for the public.
- Booklet Cardiac Arrest: Dr. Emil Levin refutes the American Heart Association's claims about animal research and human medicine. As Dr Levin shows the medical advances came from scientific observation & treatment of humans and did not rely on animal research.
- Myths of Modern Medicine: The Increase in the Human Life Span - due to Medicine or Political Social Reforms? This article explains that the great increase in human life span in the developed world (during the 19th and 20th centuries) was due to political social reforms like better sanitation systems and improved hygiene and nutrition. It was not due to pharmaceutical drugs or other medical interventions.
- Doctors Against Vivisection on Scientific & Medical Grounds (vivisection = medical research using live animals/humans). These doctors explains that vivisection is misleading and very damaging to human medicine. Furthermore, that it is not done for science but for commercial reasons to help insure companies against law suits from humans who are damaged by medical treatment.
![]()
Return to
home page:
MedicineKillsMillions
For diagrams that illustrate the decline of the major infectious diseases see the article: Truth About the Decline of the Infectious Diseases
- Why Do Pharmaceutical Drugs Injure & Kill So Many People? Are we the real guinea-pigs? Medical journals report that pharmaceutical drugs kill over 100,000 people and seriously injure millions, each year, in just the USA. Other studies claim the figures are higher. This article explains how drug companies use unscientific tests to make their products look "safe" for the public.
- Booklet Cardiac Arrest: Dr. Emil Levin refutes the American Heart Association's claims about animal research and human medicine. As Dr Levin shows the medical advances came from scientific observation & treatment of humans and did not rely on animal research.
For diagrams that illustrate the decline of the major infectious diseases see the article: Truth About the Decline of the Infectious Diseases
- Why Do Pharmaceutical Drugs Injure & Kill So Many People? Are we the real guinea-pigs? Medical journals report that pharmaceutical drugs kill over 100,000 people and seriously injure millions, each year, in just the USA. Other studies claim the figures are higher. This article explains how drug companies use unscientific tests to make their products look "safe" for the public.
- Booklet Cardiac Arrest: Dr. Emil Levin refutes the American Heart Association's claims about animal research and human medicine. As Dr Levin shows the medical advances came from scientific observation & treatment of humans and did not rely on animal research.